7 Useful Plantar Fasciitis Quick Fix & Relief Methods


What Is Plantar Fasciitis?
Plantar fasciitis is the most common cause of heel pain, affecting millions of people worldwide. Plantar fasciitis happens when the thick tissue band that links your heel to your toes becomes inflamed. It can also develop small tears. The plantar fascia supports your foot’s arch and absorbs shock, helping carry your body weight with every step.
Overuse or stress can inflame this key structure. This causes sharp pain, making each step feel like you’re stepping on something sharp. Burnaby residents with active jobs or lifestyles should learn about plantar fasciitis. Understanding it can help them treat and prevent it effectively using sports medicine.
Where Is the Plantar Fascia Located In The Body?

Image Source: Mayo Clinic
The plantar fascia is a thick band of tissue on the bottom of your foot. It starts at the inner heel. Then, it extends to the base of each toe and the ball of the foot. This structure essentially forms the foundation of your foot’s arch system.
The plantar fascia works like a shock absorber. It helps spread your body weight across your foot when you walk, run, or stand. In anatomical images, red areas often show inflammation from overuse. This is especially true where the fascia attaches to the heel bone (calcaneus).
What Does Plantar Fasciitis Feel Like? What the symptoms?


The main symptom of plantar fasciitis is sharp heel pain, usually worst with your first steps after waking up. This pain is often described as feeling like you’re stepping on a nail or sharp stone. Painful area often eases with movement as the tissue warms up. However, it tends to return after long periods of sitting or standing.
The pain levels can range from mild discomfort to severe, persistent pain that disrupts daily activities. The pain typically occurs on the bottom of the heel and may extend into the arch of the foot. After exercise or prolonged activity, the discomfort often intensifies. Some people also experience stiffness and tenderness along the bottom of the foot, particularly after periods of rest.
How Common Is Plantar Fasciitis and Who Gets It?


Plantar fasciitis is remarkably common, affecting approximately 10% of the population at some point in their lives. In Burnaby’s active community, this translates to thousands of residents who will experience this condition. The condition is particularly prevalent among:
- Athletes and runners who use the scenic trails and parks throughout Burnaby
- Working adults aged 40-65 who spend long hours on their feet
- Healthcare workers, retail employees, and construction workers – common occupations in Burnaby’s diverse economy
- Individuals with certain foot structures such as flat feet, bunion, or high arches — conditions that often overlap with plantar fasciitis due to shared structural issues in the feet.
- Those wearing unsupportive shoes like high heels
Research shows that plantar fasciitis affects people across all activity levels, from sedentary office workers to elite athletes. The condition doesn’t discriminate based on fitness level. It is a concern for all Burnaby residents, regardless of their lifestyle.
Why Did I Get Plantar Fasciitis?


or many Burnaby residents, plantar fasciitis develops due to sudden increases in physical activity without proper conditioning. This often happens when people start exercising, begin running on Burnaby’s terrain, or ramp up activity levels too quickly. When starting to use custom orthotics, ease into walking routines gradually — try Burnaby’s trails for gentle, scenic progressions.
The condition often affects people who work on hard surfaces—common in Burnaby’s fast-paced, physically demanding job market. Other contributing factors include:
- Poor running mechanics combined with inadequate athletic shoes
- Lack of proper warm-up and constant stretch routines for tight calf muscles
- Insufficient stretching and strength training
- Body movement issues such as overpronation or supination
The issue is the lower body hasn’t had time to adapt to new or increased physical stress.
What’s The Most Common History Of A Plantar Fasciitis Patient?


In most cases, plantar fasciitis affects people who recently started a new exercise routine without easing into it gradually. This patient often presents with:
- Recent increase in running or walking activity without gradual progression
- Use of old or unsuitable footwear that lacks proper support
- Neglect of proper recovery protocols including plantar fasciitis stretches and strengthening
- Poor biomechanics that haven’t been addressed
This pattern often starts when someone suddenly becomes active—like starting a standing job, exercise routine, or running. Without proper conditioning and gradual adaptation, the plantar fascia becomes overloaded and inflamed.
Even if only one left foot hurts, caring for both helps avoid imbalance and pain in the other leg.
What Are The Risk Factors of Plantar Fasciitis On Clinical Check?
During a clinical check, healthcare providers commonly identify several risk factors that increase the likelihood of developing plantar fasciitis:
Structural and Body Movement Factors:
- Flat feet (pes planus) or high arches (pes cavus) that alter normal foot mechanics
- Abnormal walking patterns or gait problems
- Weakness in gluteal and core muscles due to deconditioning
- Ankle instability and improper joint alignment
Occupational and Lifestyle Factors:
- Occupations requiring prolonged standing or walking on hard surfaces – common in Burnaby’s healthcare, retail, and construction industries
- Obesity or pregnancy which increases load on the plantar fascia — custom orthotics can help manage this extra pressure.
- Age between 40-60 years when tissues become less flexible
Footwear-Related Factors:
- Worn-out shoes with inadequate sole support
- Heavy work boots (like steel-toed boots) that require extra effort from the plantar fascia
- Lack of supportive footwear in daily routines
When Should I Consult A Doctor About My Heel Pain?


Most people with plantar fasciitis will recover within a few months using conservative treatments such as icing, stretching, and rest. However, you should make an appointment with your doctor or a podiatrist if:
- No improvement after 2 weeks of consistent home treatment
- Pain is increasing despite conservative measures
- Severe heel pain that prevents normal walking or daily activities
- Signs of complications such as numbness, tingling, or swelling
Early intervention is crucial because prolonged, untreated plantar fasciitis can lead to more serious complications and longer recovery times. Don’t wait for the condition to worsen – seeking medical help within the first few weeks can significantly improve outcomes.
What Happens If I Don’t Treat Plantar Fasciitis?


Left untreated, plantar fasciitis can lead to several serious complications:
Structural Changes:
- Degeneration at the heel attachment point where the fascia connects to the bone
- Development of bone spurs as the body attempts to stabilize the area
- Chronic inflammation that becomes increasingly difficult to treat
Functional Consequences:
- Altered gait patterns affecting joints, hips, knees, or back
- Reduced mobility and quality of life
- Chronic pain syndrome that persists for months or years
Potential Complications:
- Stress fractures in the heel bone
- Compressed nerves causing additional pain and numbness
- Plantar fascia rupture in severe cases
The good news is that with proper other treatments, most people make a full recovery without long-term complications. The key is not to ignore persistent heel pain.
Anything I Can Do At Home To Treat My Foot Pain? Any Home Remedies?


Yes! Plantar fasciitis is treatable at home, and most people fully recover without long-term damage if it’s addressed early. The foundation of home treatment includes:
Immediate Relief Measures:
- Rest and activity modification to reduce stress on the plantar fascia
- Ice therapy for rapid pain relief
- Over-the-counter painkillers and inflammatory drugs like ibuprofen
Supportive Devices:
- Heel cushions to provide extra padding and support
- Insoles and arch supports to distribute pressure more evenly
- Night splints to maintain proper stretching while sleeping
Advanced Options:
- Custom orthotics (custom shoe inserts) for more severe cases
- Proper footwear & supportive shoes with adequate arch support and cushioning
- Regular stretching and massage with a tennis ball or frozen water bottle
The key to success is consistency with your treatment plan and patience, as healing typically takes several weeks to months.
Here They Are – 7 Exercises for foot pain and Stretches To Relieve Most Cases Of Plantar Fasciitis
The following exercises and stretches form the cornerstone of plantar fasciitis treatment. Stop immediately if you experience pain during any exercise and consult your healthcare provider.
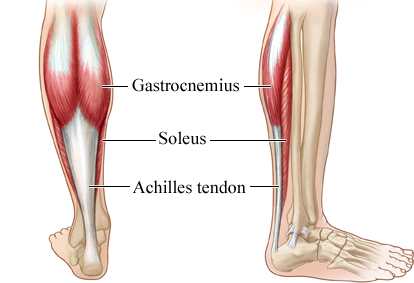
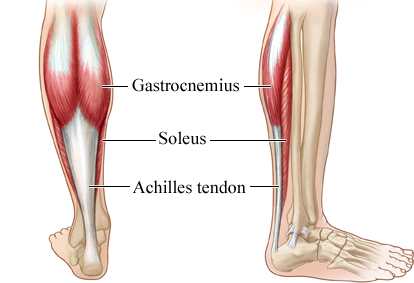
Soleus Stretch
Position your injured foot behind your uninjured foot with some space between them. Gently bend both knees until you feel a deep stretch in the calf muscle of the injured foot. This targets the deeper calf muscle that directly affects plantar fascia tension.
Hold for 20-30 seconds, repeat 3 times on both sides.
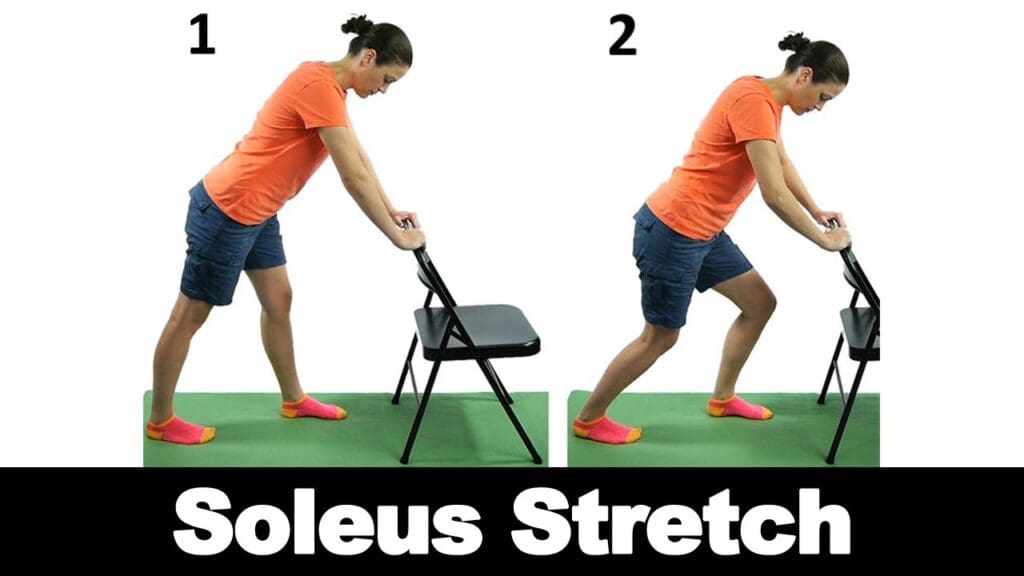
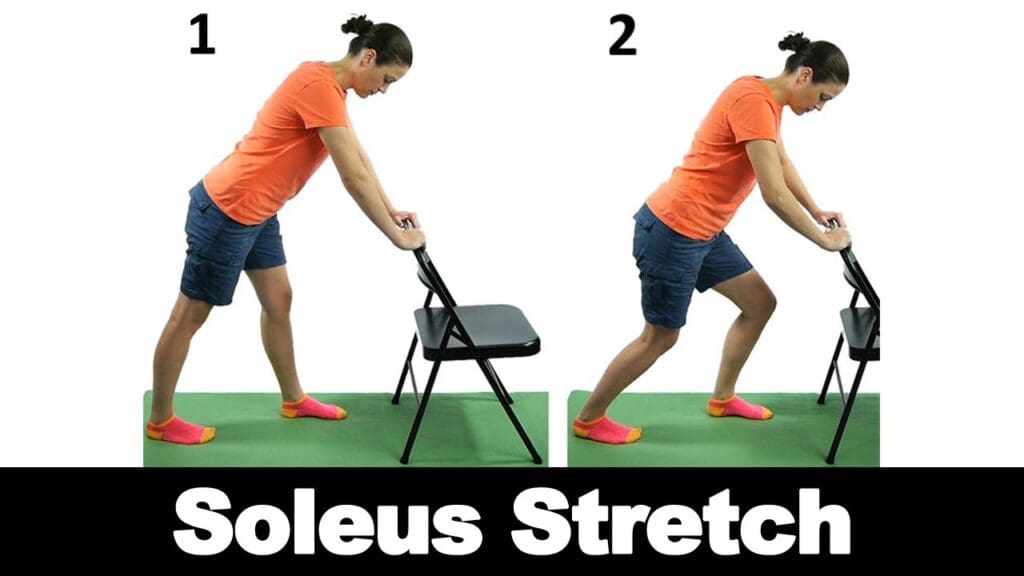
Image Source: i.timg.com
Achilles/Gastrocnemius Stretch (Calf Stretch)
Place the front of your injured foot against a wall with your heel on the floor and knee straight. “Place your hands on a wall for balance. Then slowly lean forward until you feel a stretch in your upper calf.
Hold for 20-30 seconds, repeat 3 times on both sides.


Image Source: i.pinimg.com
Plantar Fascia Stretch
Sit with legs extended, loop a towel or resistance band under the ball of your foot. Gently pull your toes toward your shin while keeping your knee straight. You should feel the stretch along the bottom of your foot and heel.
Hold for 20-30 seconds, repeat 3 times on both sides.


Image Source: hips.hearstapps.com
Towel Toe Curls
Sit with both feet flat on the floor and place a towel under your affected foot. Scrunch your toes to grab the towel, then release and relax. Focus on engaging the intrinsic muscles of your arch and feet.
Repeat 10 times for 3 sets.
Plantar Fascia Massage
Using a tennis ball or frozen water bottle, roll it under your arch and heel while sitting or standing. Apply firm pressure but avoid causing pain. The frozen water bottle provides additional anti-inflammatory benefits.
Perform for 5 minutes, 3 times daily.


Image Source: happynetty.com
Toe Extensions
Stand with your feet shoulder-width apart and engage your core. Press your heel and the ball of your foot into the ground, then lift your toes upward. This strengthens the intrinsic foot muscles and improves arch stability.
Repeat 10 times for 3 sets.
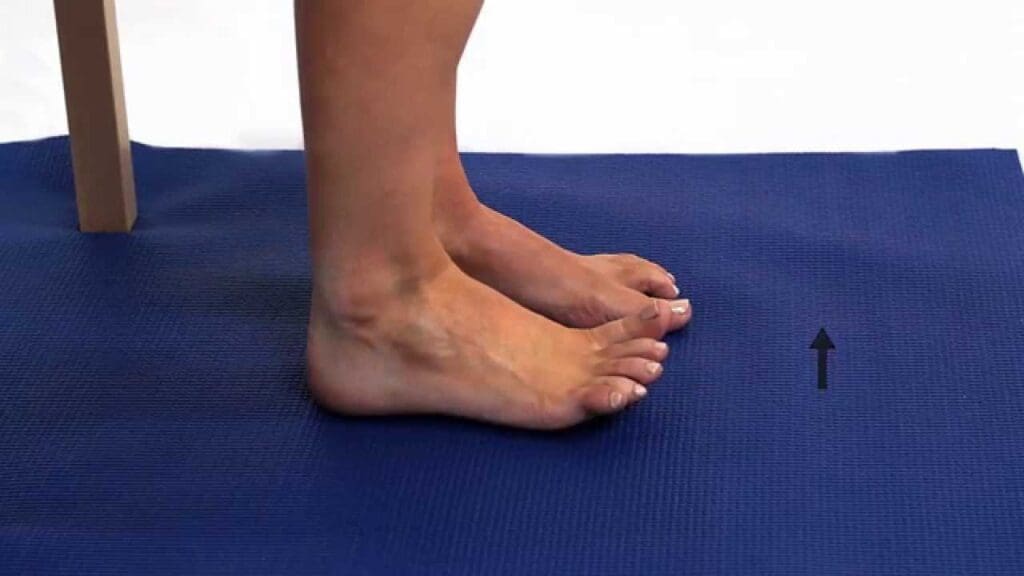
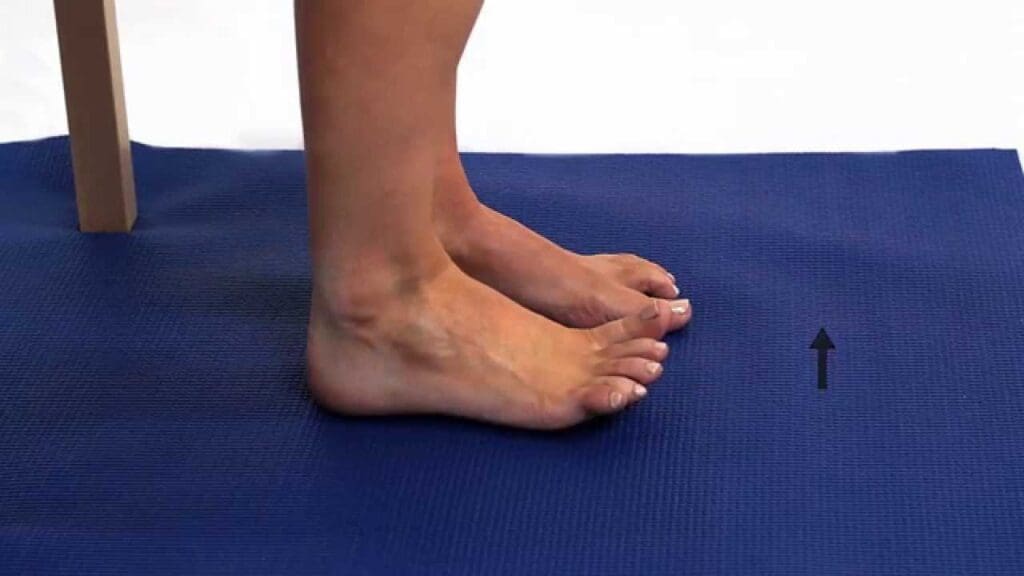
Image Source: i.timg.com
Heel Raises
Stand on the edge of a step with your heels hanging off the edge. Hold onto a wall or railing for support. Drop your heels slightly below the step level, then press up through the balls of your feet. Move slowly and controlled in a vertical direction.
Perform 10 times, 3 times daily.


Image Source: acewebcontent.azureedge.net
BONUS TIP: Marble Pickups
Sit in a chair with both feet flat on the floor. Place 20 marbles on the floor in front of you along with a small bowl. Use your toes to pick up one marble at a time and place it in the bowl. This exercise strengthens the intrinsic muscles of the foot and improves arch stability.
Repeat with both feet, aim for 20 marbles per session.
BONUS TIP: Slip on an Ice Pack
Ice therapy is highly effective for reducing inflammation and providing immediate pain relief. Apply ice for 15-20 minutes several times throughout the day, especially after activities that worsen pain. You can use:
- Ice pack slippers that mold to your foot shape
- Frozen water bottles rolled under the foot
- Frozen vegetables in a plastic bag for better conformation to foot contours
Never apply ice directly to skin – always use a thin barrier like a towel.
BONUS TIP: Try Dry Cupping
Dry cupping therapy involves placing cups on the skin to create negative pressure, which increases blood flow and reduces pain. Research shows level B evidence supporting dry cupping as effective for plantar fasciitis.
The treatment uses suction cups on targeted foot areas for 5–10 minutes to break up adhesions and boost healing. While it may leave temporary circular marks, dry cupping can be done at home with inexpensive kits.
BONUS TIP: Use Toe Separators
Toe separators help restore natural foot alignment by combating the effects of narrow, tapered shoes. These devices work by:
- Stretching shortened tendons and encouraging proper toe positioning
- Improving blood flow to the plantar fascia
- Strengthening foot muscles and improving stability
Start by wearing toe separators for 10 minutes daily during passive activities, gradually increasing to 2 hours per day10. They can be worn during exercise or even inside properly fitting shoes for enhanced benefits.
Why Is It Important to Stretch and Strengthen Both Legs?


While it’s natural to focus on the injured foot, treating both feet is crucial for several important reasons:
Preventing Compensation Patterns:
When one foot is injured, you naturally shift more weight to the healthy side, creating additional stress and strain. This compensation can lead to the healthy foot developing similar problems.
Avoiding Secondary Issues:
Altered walking patterns due to plantar fasciitis often result in hip, knee, or back problems. By maintaining strength and flexibility in both feet, you help preserve normal biomechanics.
Ensuring Balanced Recovery:
Many people develop plantar fasciitis in both feet, even if symptoms appear in only one initially. Bilateral treatment helps prevent the condition from spreading to the unaffected side.
If you’re short on time, focus on the injured foot. But it’s better to care for both feet than to ignore the problem.
Should I Try To Strengthen My Leg Muscles As Well?


Absolutely! Once you’re making progress with foot-specific exercises, incorporating lower limb strengthening can help prevent plantar fasciitis from recurring1. Strong leg muscles provide better support for your feet and improve overall biomechanics.
Recommended Strengthening Exercises:
- Squats and lunges to build leg and glute strength
- Single-leg stance activities to improve balance and proprioception
- Calf raises and step-ups to strengthen the posterior chain
Important Technique Note:
When performing these exercises, try to maintain a “short foot” position – this means engaging your arch muscles to create stability. This technique helps reduce stress on the plantar fascia while building strength.
Caution: If you experience increased foot or arch pain during strengthening exercises, stop immediately and consult your healthcare provider.


Image Source: prod.skimable
Plantar Fasciitis Treatment If Stretches/Strengthening Fails To Relieve Foot Pain?
When conservative treatments don’t provide adequate relief, several medical devices and interventions can help manage plantar fasciitis symptoms.
Shock wave therapy is an advanced treatment that uses high-energy sound waves to promote healing and reduce pain. This is often performed in specialized clinics and may require several sessions.
Airbrace / Night Splints


Image Source: orthomed.ca
One option is an air brace, which helps reduce tension in the foot and plantar fascia. Another is a night splint. Night splints are highly effective for maintaining proper foot positioning during sleep. These devices:
- Hold the plantar fascia in a lengthened position throughout the night
- Prevent the tissue from shortening while you sleep
- Reduce morning pain by maintaining flexibility
Most people sleep with their feet pointed downward, which shortens the plantar fascia and contributes to morning stiffness. Night splints counteract this by keeping your foot at a 90-degree angle.


Image Source: orthomed.ca
Custom Orthotics? Can They Help Treat Plantar Fasciitis?
Custom orthotics are often highly effective for treating plantar fasciitis symptoms. These devices work by:
- Restoring normal arch height in patients with flat feet or high arches
- Shortening the effective length of the plantar fascia
- Distributing pressure more evenly across the foot
- Providing ongoing support throughout daily activities
At Metrotown Family Chiropractic in Burnaby, we make custom orthotics for your feet. Most local insurance plans cover them. Many clinics in Burnaby offer direct billing for orthotics and chiropractic care, making it easier to access treatment without upfront costs.


Image Source: canadianfootclinic.com
Anti-inflammatories
Anti-inflammatory treatments can provide significant relief for plantar fasciitis. Options include:
- NSAIDs (ibuprofen, naproxen) for oral anti-inflammatory effects
- Topical anti-inflammatory creams applied directly to the affected area
- Corticosteroid injections for more severe cases
- Iontophoresis – using electrical current to deliver medication through the skin
A 10-14 day course of NSAIDs can help reduce both pain and inflammation.
Physical Therapy
Physical therapy takes a comprehensive approach to treating plantar fasciitis. A skilled physical therapist will:
- Assess your gait and posture to identify contributing factors
- Design personalized exercise programs for your specific needs
- Use specialized techniques like dry needling, ASTYM, or taping
- Provide footwear recommendations and movement corrections
Physical therapy is particularly beneficial because it addresses the root causes of plantar fasciitis, not just the symptoms.
Plantar Fasciitis Recovery Time
Recovery time varies significantly depending on several factors, but understanding realistic expectations can help you stay motivated during treatment. Staying consistent with your treatment helps ensure steady progress through the healing process.
Typical Recovery Timeline:
- 75% of people see improvement within 12 months without treatment
- Most people notice gradual improvement within weeks of starting treatment
- Average recovery time is 6-12 weeks with proper treatment
- Severe cases may take 8-12 weeks or longer
Factors Affecting Recovery Time:
- Early intervention leads to faster healing
- Consistency with treatment significantly impacts outcomes
- Job requirements – those with weight-bearing jobs may heal slower
- Overall health and age influence recovery speed
Important Statistics:
- Risk of ongoing symptoms is 50% after 5 years and 45.6% after 10 years in severe cases
- Only 5% of patients require surgical intervention
- Recovery is possible even in chronic cases with proper treatment
Stretches And Exercises Have Not Helped – Anything Else Can Cure Plantar Fasciitis?
When conservative treatments fail to provide relief, surgical intervention may be necessary1. However, this is required in only 5% of plantar fasciitis cases.
Surgical Options:
Plantar fascia release is a common procedure where a surgeon cuts the ligament to reduce tension, swelling, and heel pain. This is typically considered when all other efforts to cure the condition have failed. This can be performed as:
- Open surgery with a larger incision
- Endoscopic surgery using smaller incisions and specialized instruments
Success Rates:
- 70-90% success rate for plantar fascia release surgery
- 97.5% patient satisfaction in some studies
- However, only 48.8% total satisfaction in long-term follow-up studies
Important Considerations:
Recovery time typically involves 2-3 weeks before weight-bearing and 2 months for full recovery
Most surgeons recommend waiting at least 6 months before considering surgery
Extensive conservative treatment should be tried first
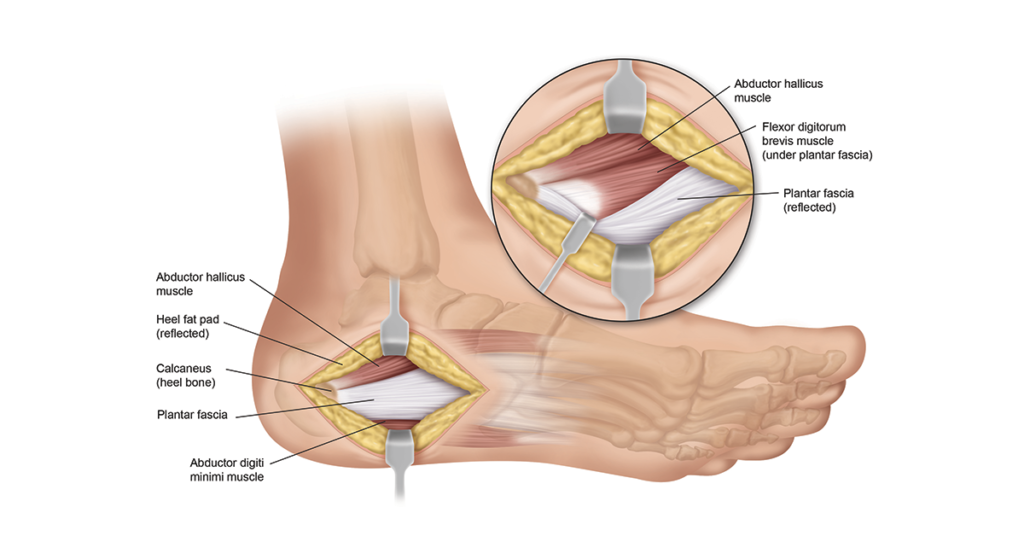
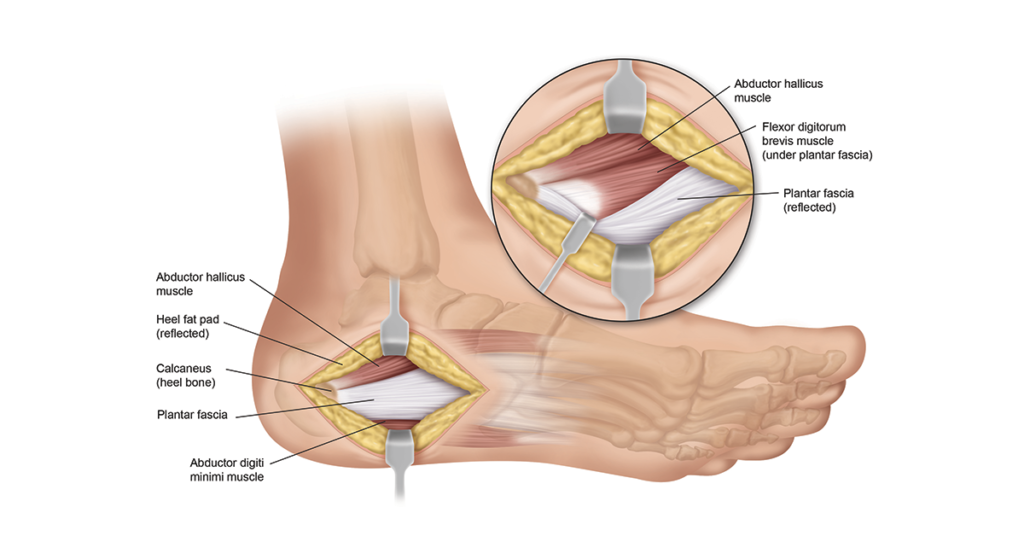
Image Source: heelthatpain.com
We Wish You Good Luck!
All of us at Metrotown Family Chiropractic and Custom Orthotics Clinic wish you a speedy recovery from plantar fasciitis. Whether through custom orthotics, physical therapy, or advice from a podiatrist, your treatment will be personalized for your recovery. We hope this guide gave you useful tips to ease pain and help you return to your active lifestyle.
Remember that healing takes time, and consistency with your treatment plan is key to success. Every step you take toward proper treatment brings you closer to pain-free living.
For specific questions about your condition or treatment, please contact your healthcare provider for personalized advice.
Ready to Seek Professional Help for Your Plantar Fasciitis?
If you’re in Burnaby and dealing with plantar fasciitis pain, reach out today for expert care and support. At Metrotown Family Chiropractic and Custom Orthotics Clinic, our experienced team specializes in treating various musculoskeletal conditions, including plantar fasciitis. We provide custom orthotics Burnaby designed to relieve plantar fasciitis and support your long-term foot health.
We offer tailored solutions to meet your individual needs, including:
- Comprehensive assessments to identify underlying causes
- Custom orthotic fitting and prescription
- Integrated treatment plans combining multiple therapeutic approaches
- Ongoing support throughout your recovery journey
Take the first step toward a pain-free life by scheduling a consultation with our Burnaby chiropractor today. Your journey to wellness begins here, and we’re committed to helping you achieve lasting relief from plantar fasciitis. Book your consultation today and take the first step toward walking comfortably again.